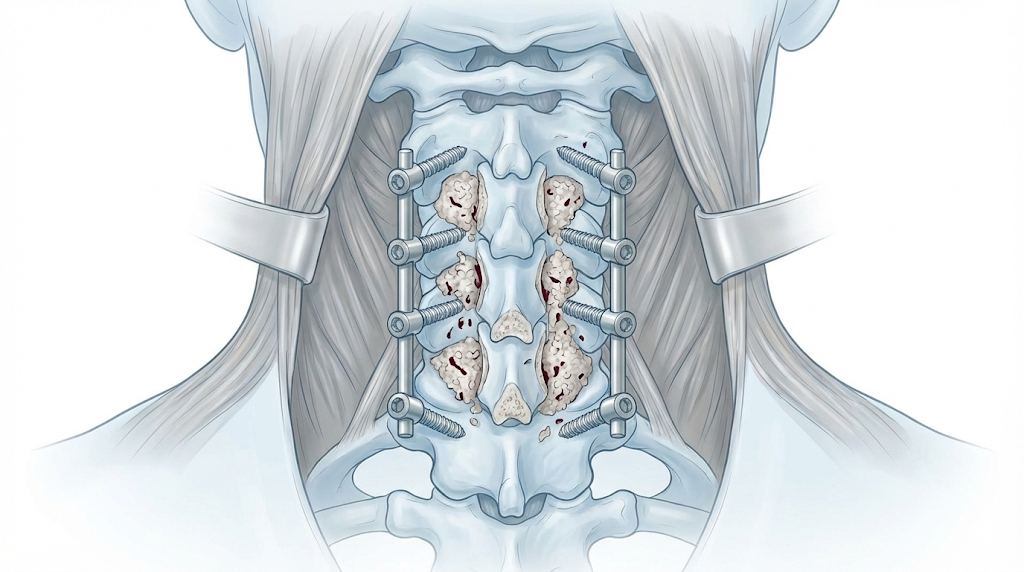
Posterior cervical fusion (instrumentation with lateral mass or cervical pedicle screws)
Posterior cervical fusion (instrumentation with lateral mass or cervical pedicle screws) is considered for patients with chronic neck pain, stiffness and often arm radiation or difficulty walking and balancing. Most have tried medication, physiotherapy or other conservative measures without sufficient improvement and imaging shows instability, deformity or posterior compression. The procedure decompresses the cord and nerve roots and stabilises multiple levels from the back of the neck using screws, rods and bone graft, providing strong fixation. Indication is personalised, based on symptoms, neurological exam and MRI/CT to protect neurological function and slow progression.
What is Posterior cervical fusion?
Posterior cervical fusion is a stabilisation procedure performed from the back of the neck. Screws are placed in the lateral masses or pedicles, connected with rods, and bone graft is added to achieve solid fusion, correcting or preventing instability and protecting the cord and roots. It also allows wide posterior decompressions such as laminectomy or foraminotomy when needed.
Symptoms and warning signs
Watch for:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
A detailed neurological exam and thorough imaging review define which levels need decompression and fixation. Goals, approach, alternatives and risks are explained, addressing questions. Fasting instructions and medication adjustments (especially anticoagulants and antiplatelets) are given, and comorbidities are assessed with anaesthesia before consent.
2.During the procedure
Under general anaesthesia, the patient is usually positioned prone with the head secured. A midline posterior incision exposes the bone. Screws are placed in the lateral masses or pedicles, guided by anatomical landmarks, intraoperative imaging and sometimes navigation. Laminectomy or foraminotomy may be performed to decompress the cord and roots. Rods are connected, bone graft is added to promote fusion and the wound is closed, with a drain if needed.
3.Immediate postoperative period
After surgery, vitals, neurological status and pain are monitored in recovery and then on the ward. Muscle pain in the back of the neck and shoulders is common and managed with analgesia. Mobilisation starts gradually (sitting, standing, walking), often within the first 24–48 hours. Hospital stay is typically 3–5 days depending on pain, strength, gait and wound progress.
Recovery and daily life
Recovery is progressive and can be slower than anterior approaches due to posterior muscle dissection. Early weeks often bring muscle pain, fatigue and neck stiffness. Basic activity starts early while avoiding effort, lifting and sudden movements. Return to office work is usually considered between 4 and 6 weeks; physical or high-risk jobs may need 3–4 months or more. Physiotherapy, strengthening and posture correction are key. If fever, marked swelling, worsening pain, new weakness or gait change appears, prompt review is required.
Risks and possible complications
General risks: complications of general anaesthesia, wound infection, bleeding, haematoma and venous thrombosis. Specific risks: spinal cord or nerve root injury with possible worsening strength or sensation; lack of bone fusion (pseudoarthrosis); screw malposition that may require revision; residual or chronic neck pain; progression of degeneration at adjacent segments and risk of deformity if alignment is not maintained. These risks are always weighed against leaving significant stenosis or instability untreated.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala