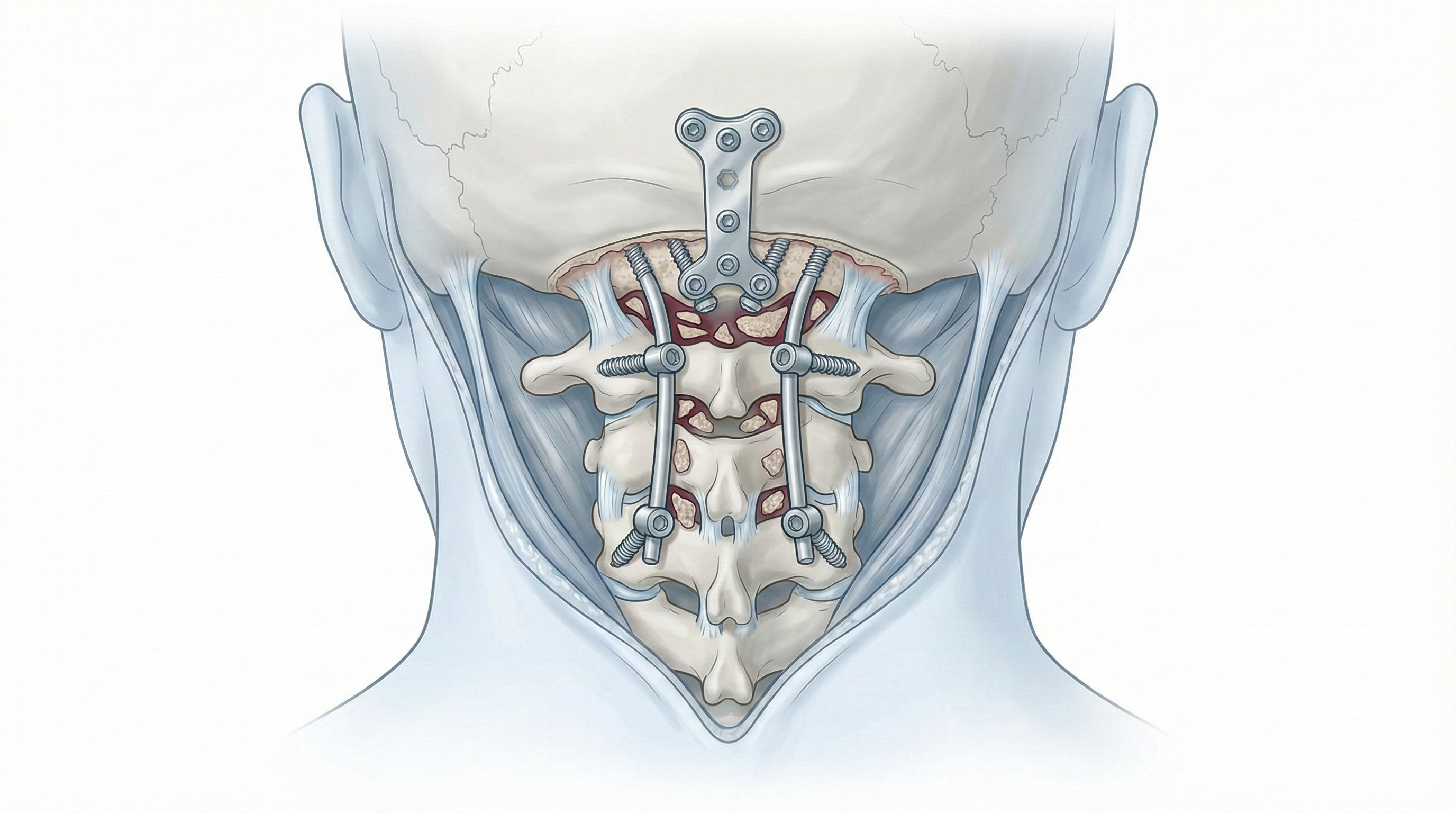
Occipitocervical fusion (occipital to upper cervical spine)
Occipitocervical fusion (occipital to upper cervical spine) is indicated for patients with severe upper-neck and occipital pain, instability or difficulty keeping the head upright, often with neurological symptoms (tingling, weakness, gait issues) from cord compression at the craniocervical junction. The procedure rigidly connects the occipital bone to the upper cervical vertebrae using screws, rods and bone graft to create a stable construct that protects the cord and nerve roots. Indication is personalised, based on symptoms, neurological exam and MRI/CT, especially in complex scenarios such as instability, deformity, trauma or inflammatory disease.
What is Occipitocervical fusion?
It is a stabilisation surgery that links the occipital bone to the upper cervical vertebrae (usually C1–C2) with instrumentation and bone graft to prevent unstable motion that could compress the cord or roots. Unlike other cervical fusions, it targets the craniocervical junction, a highly mobile area close to the brainstem.
Symptoms and warning signs
In craniocervical conditions, watch for:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
A thorough neurological exam and detailed review of MRI, CT and dynamic X-rays are performed. Goals, instrumentation, benefits and risks are explained. Fasting instructions and adjustments of anticoagulants/antiplatelets are given, with comorbidities assessed by anaesthesia. Additional studies may be requested in complex anatomy.
2.During the procedure
Under general anaesthesia, the patient is positioned prone with the head secured. A midline occipital–cervical incision exposes the occipital bone and upper cervical vertebrae. Occipital anchors and cervical screws (lateral mass or pedicle) are placed, with decompression (laminectomy) if needed. They are connected with rods, bone graft is added for fusion and the wound is closed in layers with a drain if needed.
3.Immediate postoperative period
After surgery, vitals, neurological status and pain are monitored in recovery and on the ward. Neck and occipital pain is expected and managed with analgesia. Mobilisation starts progressively (sitting, walking with assistance). A cervical collar is often used to protect early fusion. Hospital stay is usually 4–7 days depending on recovery.
Recovery and daily life
Recovery is gradual and requires adapting to reduced neck motion. Early weeks often bring muscle pain, fatigue and limited movement. Return to office work is usually considered between 6 and 8 weeks; physical or high-risk jobs may need 3–6 months or more. Physiotherapy, posture re-education and tailored exercises build strength and balance. Watch for fever, swelling, new weakness, gait or sensory changes and seek prompt review if they occur.
Risks and possible complications
General risks: anaesthesia, infection, bleeding, haematoma, venous thrombosis. Specific risks: spinal cord or root injury with neurological worsening, malposition of screws or anchors requiring revision, pseudoarthrosis, residual or chronic neck pain, loss of neck mobility, adjacent level degeneration and, rarely but importantly, vascular injury or damage near the brainstem. These risks are weighed against leaving severe occipitocervical instability untreated.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala