Expansive cervical laminoplasty
Expansive cervical laminoplasty is considered for patients with neck pain, stiffness and arm or hand symptoms from cervical stenosis compressing the spinal cord. When medication, physiotherapy or injections are no longer sufficient, it allows wide canal decompression. The procedure opens the laminae through a posterior approach, creating a “door” that is fixed in a wider position with plates or sutures to give the cord more space while aiming to preserve stability and some motion. Indication is personalised after neurological examination and imaging, weighing expected benefits, recovery and risks before deciding.
What is expansive cervical laminoplasty?
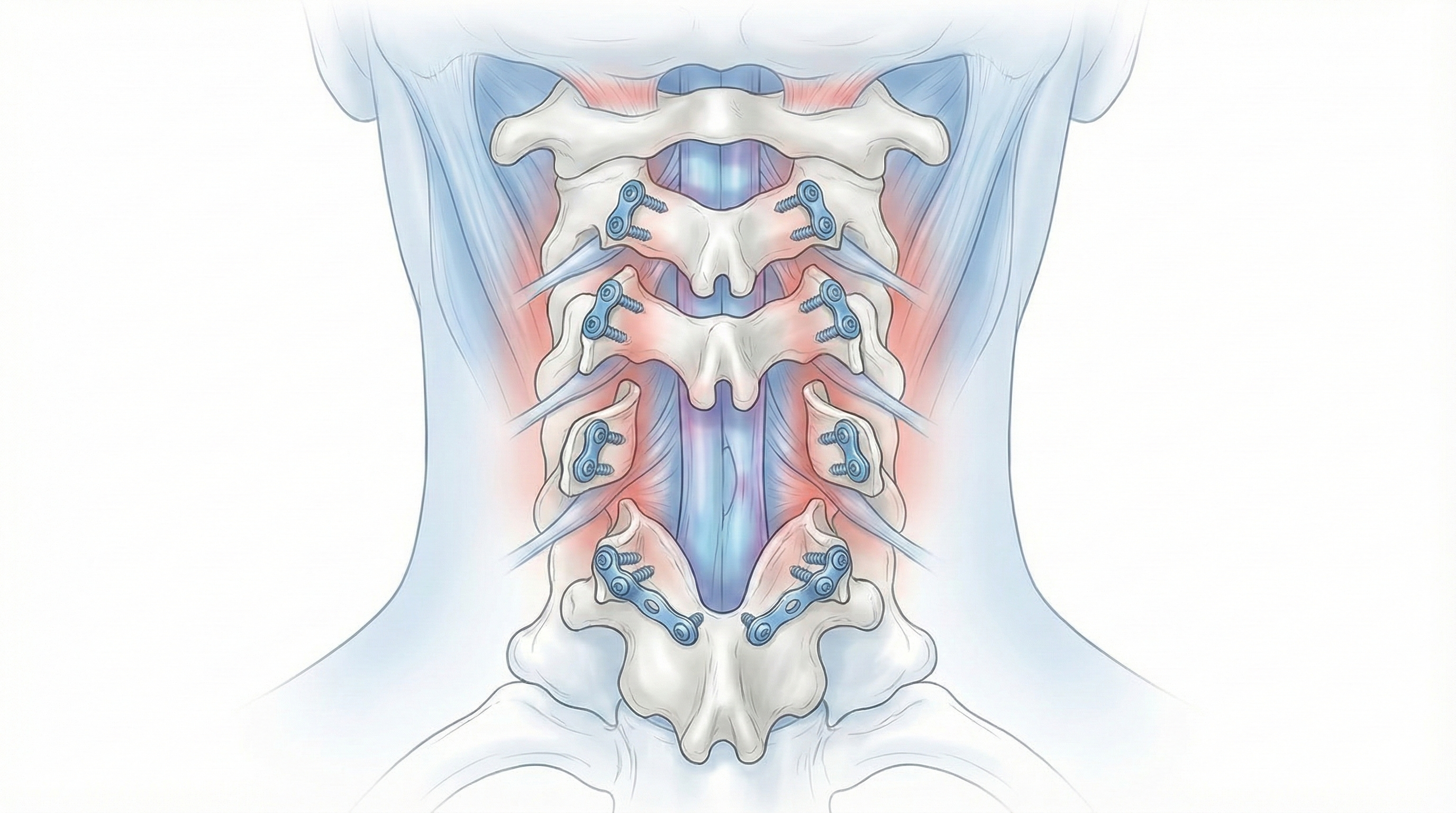
Expansive cervical laminoplasty is a surgical technique in which the back part of the cervical spinal canal (the laminae) is opened and “expanded” to create more space for the spinal cord without completely removing the bone. Controlled cuts are made to create a “door” that is fixed in a wider position, usually with small plates or sutures, so the canal enlarges. This procedure acts on the posterior laminae and spinal canal without fully removing the back of the vertebra. The goal is to decompress the spinal cord when diffuse compression is caused by arthritis, ossification or multilevel stenosis. Unlike techniques such as simple laminectomy or some posterior fusions, expansive cervical laminoplasty aims to preserve stability and some motion, reducing the risk of deformity over time in selected patients.
Symptoms and warning signs
Patients who may benefit from expansive cervical laminoplasty often show signs of cervical myelopathy and sometimes radiculopathy. It is important to pay attention to:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
Before expansive cervical laminoplasty, a thorough clinical assessment is performed, focusing on neurological examination and balance. Imaging studies are reviewed in detail to define the levels to treat. The neurosurgeon explains the goal of surgery, the technique, expected benefits and potential risks, answering all patient questions. Fasting instructions are given, medication is reviewed (especially blood thinners or antiplatelets) and hospital admission is organised. Once everything is clarified, informed consent is signed.
2.During the procedure
Expansive cervical laminoplasty is performed under general anaesthesia through a posterior approach. Muscles are separated to expose the laminae of the cervical vertebrae to be treated. Controlled cuts create a “door” that opens to one side, enlarging the spinal canal. The laminae are fixed in their wider position using small plates, screws or special sutures so the canal remains expanded and the cord has more space. Decompression is checked and the wound is closed in layers.
3.Immediate postoperative period
After surgery, the patient spends time in recovery to monitor awakening from anaesthesia, breathing and pain control. Then they return to the ward, where progressive mobilisation usually starts the next day. Strength, sensation, gait and neck pain are closely monitored. Hospital stay typically lasts 2–3 days, adjusted to each patient’s progress.
Recovery and daily life
In the first days after expansive cervical laminoplasty, neck pain, stiffness and fatigue are common. Basic mobilisation (getting up, short walks, personal hygiene) usually begins early. Returning to office work is often considered between 4 and 6 weeks if recovery is favourable. For physical jobs involving lifting or forced neck postures, recovery is typically 8–12 weeks or more depending on individual response and job demands. Physiotherapy, gait retraining, progressive strengthening of cervical and dorsal muscles, and ergonomic habits are essential. If fever, intense pain that does not improve, new weakness, worsening gait or any alarm symptom appears, contact the specialist for reassessment.
Risks and possible complications
As with any spine surgery, expansive cervical laminoplasty carries risks, although most patients recover satisfactorily. Knowing them helps make a balanced decision. General risks include anaesthesia-related problems, wound infection, bleeding, haematoma formation and venous thrombosis. Specific risks include nerve root or spinal cord injury, persistent cervical muscle pain, lack of neurological improvement, insufficient canal widening, displacement or failure of fixation material and changes in cervical alignment. Some patients may also experience shoulder or neck discomfort related to posterior muscles. Although uncommon, these risks must be weighed against the severity of stenosis and the patient’s symptoms. The decision is always individual.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala