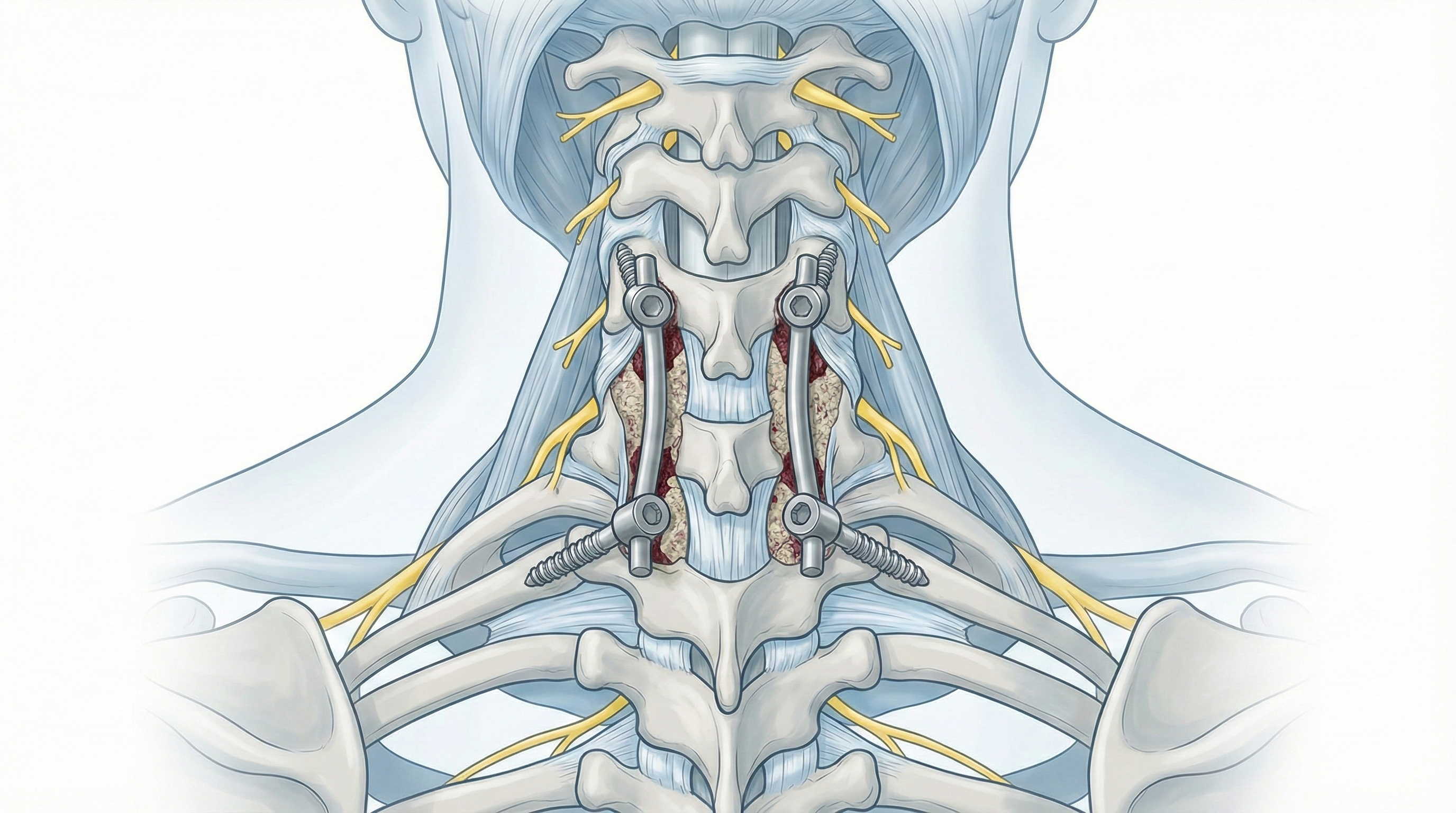
Cervicothoracic fusion (fixation from lower cervical to thoracic spine)
Cervicothoracic fusion (fixation from lower cervical to thoracic spine) is considered for patients with lower neck and upper back pain, instability or forced head posture unresponsive to medication or physiotherapy, with imaging showing deformity, stenosis or compression at the cervical–thoracic junction. Using screws and rods that connect lower cervical and upper thoracic vertebrae, plus bone graft and decompression when needed, the goal is to protect the cord and roots and provide lasting stability. Indication is personalised after assessing symptoms, neurological exam and MRI/CT, especially in complex deformity, post-traumatic changes or advanced stenosis.
What is Cervicothoracic fusion (fixation from lower cervical to thoracic spine)?
It is a stabilisation surgery linking the lower cervical vertebrae (usually C6–C7) to one or more upper thoracic levels with screws, rods and bone graft to create a stable construct. Decompression (laminectomy, foraminotomy) is often combined when there is stenosis or cord/root compression.
Symptoms and warning signs
Watch for:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
A full neurological assessment and detailed review of MRI, CT and X-rays (including dynamic studies when needed) define levels to decompress and fix. Goals, instrumentation, potential combined approaches and risks are explained. Fasting instructions, anticoagulant/antiplatelet adjustments and comorbidity assessment with anaesthesia are provided.
2.During the procedure
Under general anaesthesia, a posterior approach is usually used with the patient prone and the spine aligned. A midline incision over lower cervical and upper thoracic levels allows placement of screws guided by anatomy and imaging. Decompression of cord and roots (laminectomy, foraminotomy) is performed if needed. Rods are connected, bone graft is added for fusion and alignment is checked before layered closure, with a drain if required.
3.Immediate postoperative period
After surgery, vitals, neurological status and pain are monitored in recovery and on the ward. Neck and upper-back pain is expected and managed with analgesia. Mobilisation begins gradually (sitting, walking with assistance). A collar or brace may be used depending on stability. Hospital stay is usually 4–7 days depending on neurological progress, pain and overall status.
Recovery and daily life after cervicothoracic fusion
Recovery is progressive and may take months. Early on, muscle pain, stiffness and fatigue with posture are common. Basic activity starts early while avoiding effort, sudden twists and heavy lifting. Return to office work is often considered between 4 and 8 weeks; physical or high-risk jobs may require 3–6 months or more. Physiotherapy, guided rehab and ergonomics are key to regaining function and protecting the spine. Watch for fever, wound discharge, severe pain, new weakness or sensory changes and seek prompt review if they occur.
Risks and possible complications
General risks: anaesthesia, infection, bleeding, haematoma, venous thrombosis. Specific risks: spinal cord or root injury with worsening strength or sensation; screw malposition that may need reoperation; pseudoarthrosis at fused levels; persistent chronic pain; progression of degeneration at adjacent segments; potential alteration of overall alignment if not properly corrected. These risks are weighed against leaving significant cervicothoracic stenosis or instability untreated.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala