Cervical foraminotomy (anterior or posterior approach)
Cervical foraminotomy (anterior or posterior approach) is considered for patients with neck pain radiating to the shoulder and arm, often with tingling or weakness caused by nerve root compression in the foramen. When medication, physiotherapy or injections are no longer enough and imaging shows foraminal narrowing or a lateral disc herniation, this surgery frees the nerve via an anterior or posterior approach depending on where the compression is. The goal is to relieve radicular pain while preserving segment stability and motion as much as possible, with indication always personalised based on symptoms and imaging.
What is Cervical foraminotomy (anterior or posterior approach)?
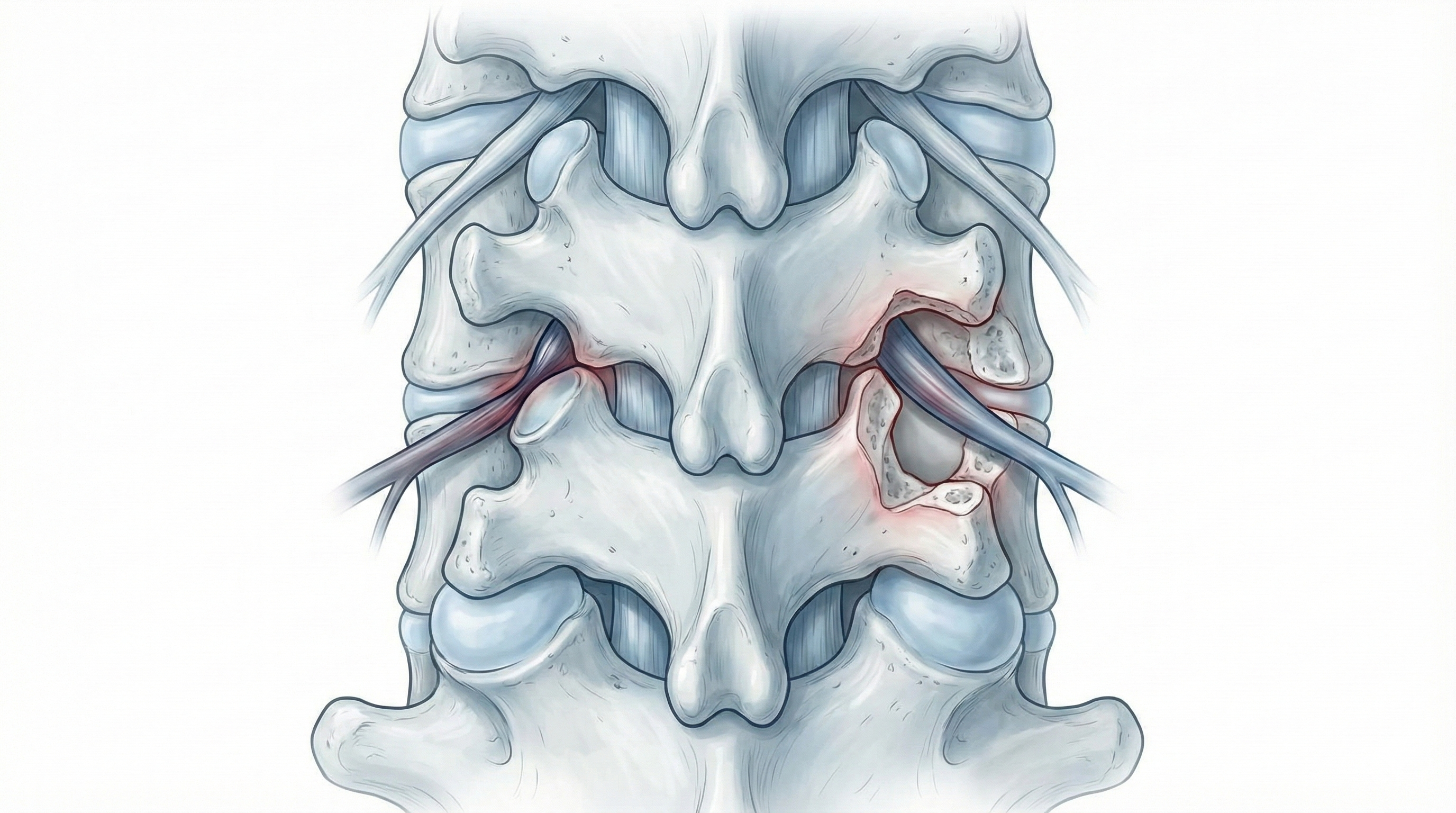
Cervical foraminotomy (anterior or posterior approach) is a surgical procedure to enlarge the cervical foramen, the bony canal where the nerve root exits to the arm, when it is compressed by disc herniation, arthritis, thickened ligaments or other degenerative changes. It can be performed through an anterior approach, reaching the disc and foramen from the front of the neck, or through a posterior approach, creating a small bone “window” around the nerve. The choice depends on compression location, anatomy and clinical factors. Unlike wider decompressions or fusions, foraminotomy targets the affected foramen to relieve radicular pain while preserving as much stability and motion as possible.
Symptoms and warning signs
Patients who may benefit typically show cervical radiculopathy symptoms:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
A full clinical assessment is performed with targeted neurological exam and detailed imaging review to locate the affected root. The neurosurgeon explains the goal, proposed approach (anterior or posterior), alternatives and risks. Fasting instructions are given, medication is reviewed—especially blood thinners or antiplatelets—and hospital admission is planned before signing consent.
2.During the procedure
Under general anaesthesia, foraminotomy can be done via an anterior approach with a small neck incision to reach the disc and foramen, removing compressive material (disc fragments or bone spurs) and enlarging the space; in some cases additional disc or stabilisation steps are performed. Via a posterior approach, an incision in the back of the neck allows selective removal of a small amount of bone and ligament around the foramen to free the root. Intraoperative imaging is used in both approaches to confirm localisation.
3.Immediate postoperative period
After surgery, patients spend time in recovery to monitor awakening from anaesthesia, breathing and pain control, then return to the ward. Mobilisation usually starts early, the same day or next, beginning with getting up and short walks. Strength, sensation and radicular pain are monitored. Hospital stay is typically 24–48 hours, tailored to recovery.
Recovery and daily life
Neck discomfort and some stiffness are common in the first days. Basic mobilisation starts early. Return to office work is often considered between 2 and 3 weeks if pain is controlled; physical jobs with lifting, repetitive shoulder or neck movements, or forced postures usually require 4 to 6 weeks or more depending on recovery. Physiotherapy, progressive strengthening of cervical and shoulder muscles, workplace ergonomics and healthy habits help maintain results. If fever, severe pain, new weakness or worsening tingling appears, prompt review is advised.
Risks and possible complications
As with any spine surgery, cervical foraminotomy (anterior or posterior) carries risks. General risks include anaesthesia-related issues, wound infection, bleeding, haematoma and venous thrombosis. Specific risks include nerve root injury, persistence or lack of pain improvement, segmental instability if too much bone is removed, residual neck pain, and with the anterior approach, temporary swallowing difficulty or voice changes; posterior approach may cause neck muscle pain. These risks are weighed against expected benefits in each case.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala