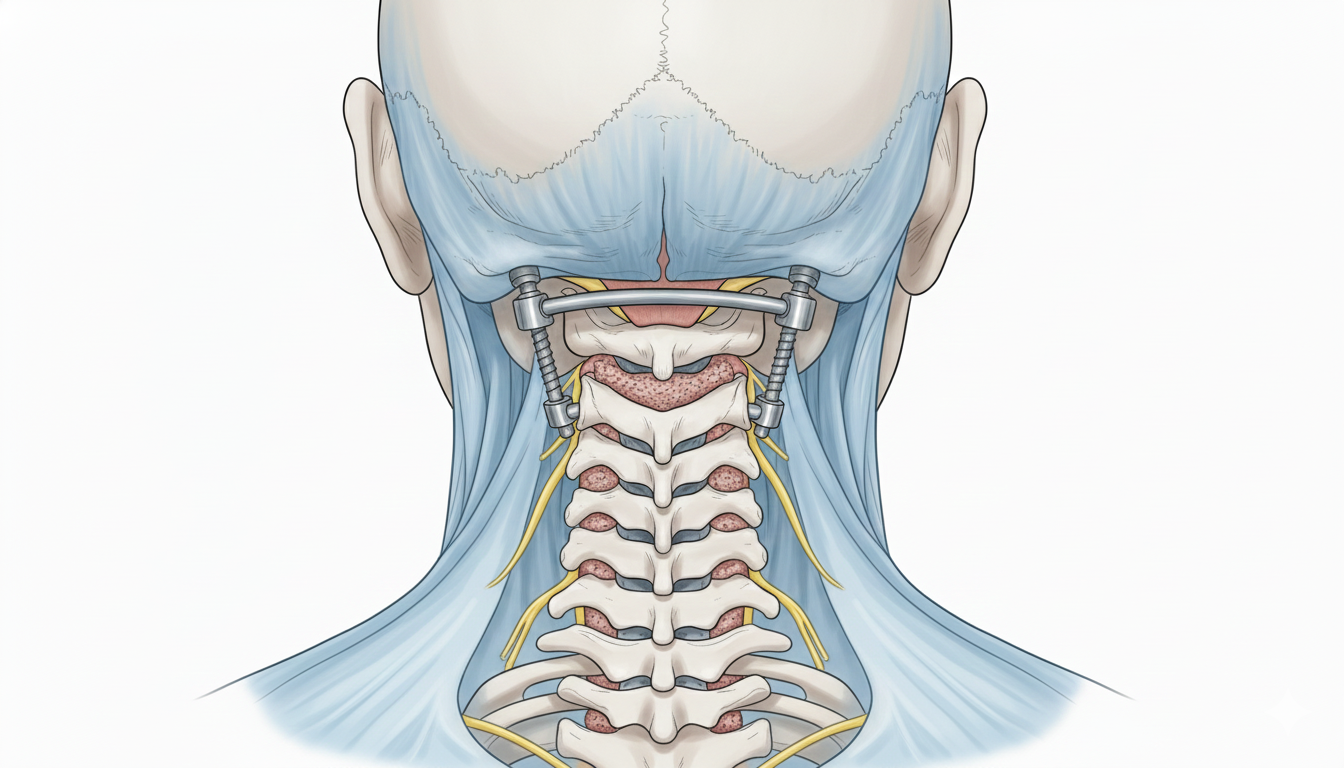
C1–C2 atlantoaxial fusion
C1–C2 atlantoaxial fusion is considered for patients with high neck and occipital pain, instability or difficulty keeping the head steady, often with tingling, weakness or gait issues from cord compression at the C1–C2 joint. Using screws and rods to fix the atlas and axis, plus bone graft, it aims to stabilise the upper cervical spine and protect the cord and roots. Indication is personalised based on symptoms, neurological exam and imaging when instability or disabling pain do not respond to conservative measures.
What is C1–C2 Atlantoaxial Fusion?
It is an upper cervical fusion linking the atlas (C1) and axis (C2) with screws, rods and bone graft to eliminate unstable motion that can cause pain or compress the cord and roots. It is performed through a posterior approach to stabilise the atlantoaxial joint.
Symptoms and signs to consider
In C1–C2 instability, watch for:
When is this surgery indicated?
Step-by-step overview of the procedure
1.Preoperative evaluation and planning
Neurological exam and detailed review of MRI, CT and X-rays (including dynamic studies) confirm instability and guide screw planning. Goals, benefits and risks are explained, medication (anticoagulants/antiplatelets) is adjusted and fasting instructions are provided before admission.
2.Screw and rod placement and fusion preparation
Under general anaesthesia via a posterior approach, the patient is positioned prone with the head secured. C1 and C2 are exposed, screws are placed in C1 lateral mass and in C2 (pedicle or pars) as anatomy allows, guided by landmarks and imaging. Rods are connected, bone graft is placed to promote fusion and stability is checked before closing the wound.
3.Immediate postoperative care and early mobilisation
After surgery, vitals, pain and neurological status are monitored in recovery and on the ward. Upper neck pain is expected and managed with analgesia. Mobilisation usually starts gradually (sitting, walking with assistance), and a collar may be used depending on the team’s criteria. Typical hospital stay is 48–72 hours if recovery is favourable.
Recovery and daily life after C1–C2 fusion
Recovery is gradual. Early weeks often bring muscle pain and stiffness, improving with analgesia and physiotherapy. Effort and abrupt neck movements should be avoided. Return to office work is usually considered between 3 and 4 weeks; physical jobs may need 8–12 weeks or more. Follow rehab guidance and watch for red flags such as fever, increased pain, weakness or sensory changes.
Risks and possible complications
General risks: anaesthesia, wound infection, bleeding, haematoma, venous thrombosis. Specific risks: spinal cord or root injury with neurological worsening, screw malposition requiring revision, pseudoarthrosis, residual neck pain, loss of cervical rotational mobility and, rarely, vascular injury. These risks are weighed against the benefit of stabilising C1–C2 in each case.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala