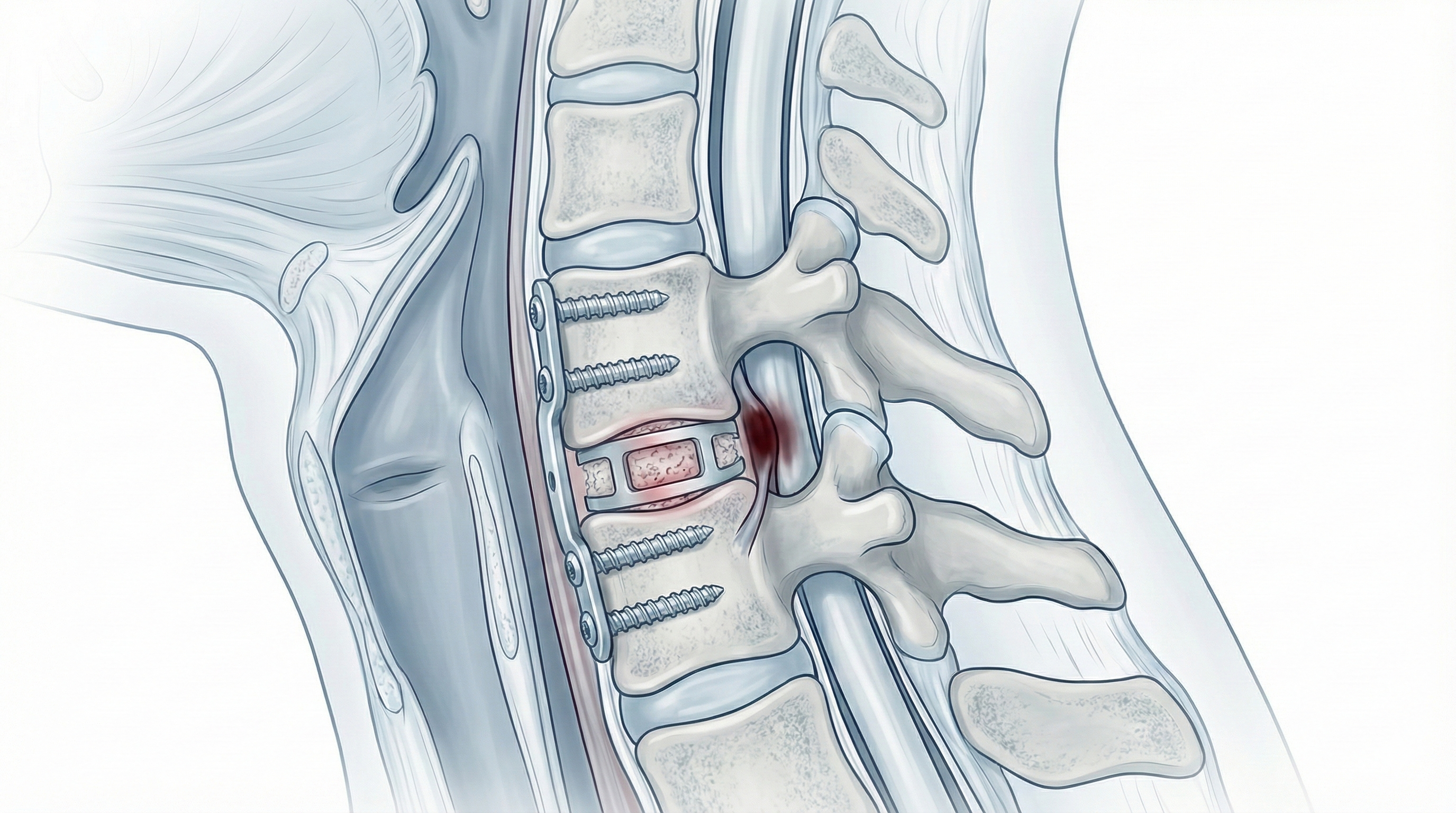
Anterior cervical fusion (interbody fusion with plate)
Anterior cervical fusion (interbody fusion with plate) is considered for patients with neck pain radiating to the arm, tingling or weakness after months of persistent symptoms despite conservative care and imaging showing a degenerated or herniated disc compressing the root or cord. Through a small incision at the front of the neck, the diseased disc and bone spurs are removed, a cage or graft is placed to maintain height and promote fusion, and a plate with screws provides stability. The goal is to relieve nerve compression and reduce painful motion at that segment, with indication always personalised to symptoms and imaging.
What is Anterior cervical fusion (interbody fusion with plate)?
Anterior cervical fusion (interbody fusion with plate) combines decompression of neural structures with stabilisation of the affected segment. Through a small anterior neck approach, the diseased disc and compressive bone are removed and replaced with an interbody cage or graft to maintain height and allow fusion. A plate with screws on the anterior vertebrae reinforces stability. Unlike discectomy without fusion, it provides added stability, useful in markedly degenerated or unstable segments or when multiple levels are treated.
Symptoms and warning signs
In degenerative cervical disease, watch for:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
A full neurological exam and detailed imaging review confirm correlation between symptoms and affected levels. The neurosurgeon explains goals, alternatives, benefits and risks. Fasting instructions are given, medication is adjusted (anticoagulants, antiplatelets and chronic treatments) and medical history is reviewed with anaesthesia before consent.
2.During the procedure
Under general anaesthesia, a small incision on one side of the neck allows gentle separation of tissues to the cervical spine. The diseased disc and compressive osteophytes are removed, the interbody space prepared and a cage or graft inserted to maintain height and promote fusion. A plate with screws is fixed to the treated vertebrae for immediate stability. Intraoperative imaging and a surgical microscope are often used for precision.
3.Immediate postoperative period
After surgery, the patient stays in recovery for monitoring of vital signs, breathing and pain, then returns to the ward. Neck discomfort and a sore throat feeling are common initially. Mobilisation usually starts early, the same day or next, with assistance. Hospital stay is typically 24–48 hours depending on pain control, ability to eat and neurological stability.
Recovery and daily life
Recovery is often relatively quick compared to more extensive spine surgery. In the first days, neck pain, tightness and swallowing discomfort are common and usually improve. Basic activity starts early, avoiding sudden neck movements and heavy lifting. Return to office work is often considered between 2 and 3 weeks; physical or demanding jobs may require 6–8 weeks or more. Targeted physiotherapy, ergonomic advice and gentle exercises help strengthen neck muscles. If fever, marked wound redness, disproportionate pain or new weakness appears, prompt review is needed.
Risks and possible complications
As with any surgery, there are risks. General risks include anaesthesia-related issues, wound infection, bleeding, haematoma and venous thrombosis. Specific risks include nerve root injury or, less commonly, spinal cord injury, partial persistence of symptoms, transient dysphagia, injury to oesophagus, trachea, vessels or recurrent nerve, lack of bone fusion (pseudoarthrosis) and long-term adjacent level degeneration. Some residual neck pain may persist. These risks are weighed against the benefit of decompressing and stabilising the segment in each case.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala