Spinal cord decompression for cervical myelopathy
Spinal cord decompression for cervical myelopathy (including cases due to ossification of the posterior longitudinal ligament, OPLL) is considered for patients with gait difficulty, hand clumsiness, tingling and neck stiffness from sustained cord compression. When symptoms progress and medication, physiotherapy or posture measures are no longer enough, decompressing the cord aims to protect neurological function and slow deterioration. It can be performed through anterior, posterior or combined approaches depending on the stenosis pattern and OPLL, with indication always personalised to clinical findings and imaging.
What is Spinal cord decompression for cervical myelopathy?
Spinal cord decompression for cervical myelopathy (e.g. due to ossification of the posterior longitudinal ligament – OPLL) includes techniques to enlarge the space for the cord in the cervical spine and relieve pressure. Compression may result from advanced arthritis, disc herniations, thickened ligaments or OPLL forming a rigid plate that narrows the canal. Depending on the case, the approach may be anterior, removing disc or vertebral bone, posterior (laminectomy, laminoplasty) or combined, always aiming to free the cord and nerve roots. Unlike surgeries focused on a single nerve root, this decompression addresses global cord involvement seen in multilevel stenosis and OPLL, with the goal of protecting neurological function over time.
Symptoms and warning signs
Cervical myelopathy often progresses insidiously. Watch for:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
A detailed clinical and neurological assessment is performed with thorough MRI/CT review to define levels, stenosis pattern and strategy (anterior, posterior or combined). The neurosurgeon explains goals, alternatives and risks and answers questions. Fasting instructions are given, medication is reviewed (anticoagulants, antiplatelets and chronic treatments) and comorbidities are assessed with anaesthesia before signing consent.
2.During the procedure
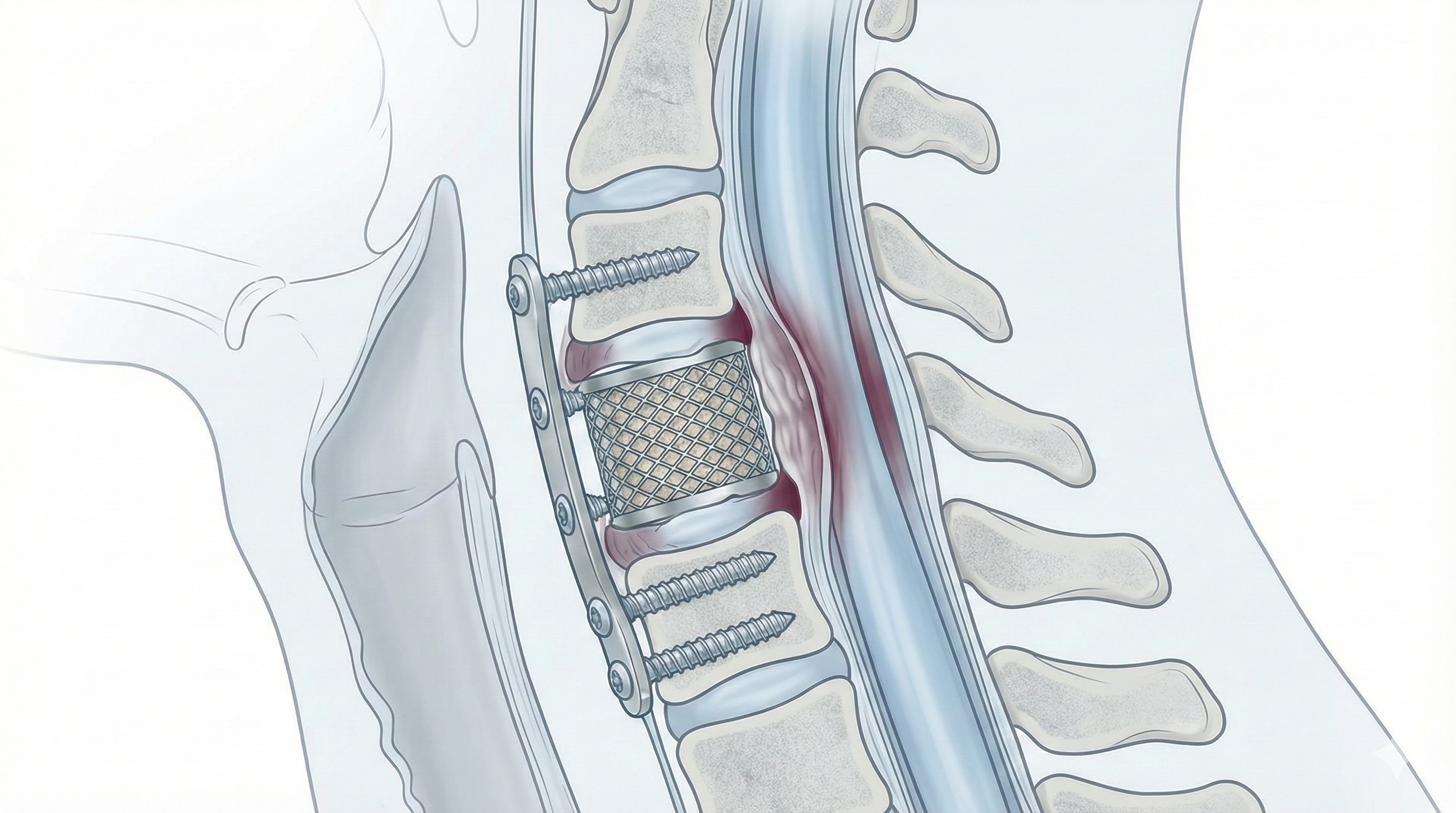
Under general anaesthesia, decompression can be performed anteriorly, removing degenerated discs, bone fragments or OPLL compressing the cord and placing cages or grafts with plates and screws for stability. Posteriorly, laminectomy or laminoplasty widens the canal from behind and, if needed, fixation with screws and rods is added. In some cases both approaches are combined to achieve complete decompression and sufficient stability.
3.Immediate postoperative period
After surgery, the patient stays in recovery where breathing, blood pressure, neurological status and pain are monitored. Then they return to the ward, with regular checks of strength, sensation and gait. Mobilisation usually begins the next day with physiotherapy. Typical hospital stay is 3–5 days, adjusted to complexity, neurological course and comorbidities.
Recovery and daily life
Recovery is usually gradual. In the first days, neck pain, fatigue and some gait insecurity are common; basic mobilisation starts early under supervision. Neurological improvement may be progressive and sometimes partial: the main goal is to slow myelopathy progression and recover function when possible. Return to office work is often considered between 6 and 8 weeks; physical or demanding jobs may require 3–4 months or more. Physiotherapy, gait retraining, cervical and dorsal strengthening and daily ergonomics are essential. If fever, severe pain, new weakness or sudden gait worsening occurs, prompt review is needed.
Risks and possible complications
As with any spine surgery, especially when involving the cord, there are risks. General risks include anaesthesia-related problems, infection, bleeding, haematoma and venous thrombosis. Specific risks include spinal cord or nerve root injury that could worsen strength or sensation, persistence or lack of myelopathy improvement, instability if not stabilised adequately, pseudoarthrosis when fusion is performed, residual or chronic neck pain and, in OPLL, technical difficulty removing rigid bone plates adherent to the cord. Long-term cervical alignment changes may also occur. These risks are weighed against the risk of neurological progression without surgery.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala