Cervical laminectomy
Cervical laminectomy is considered for patients with neck pain, stiffness and arm or hand symptoms such as tingling or weakness due to cervical stenosis compressing the spinal cord and roots. When medication, physiotherapy or injections no longer control progressing symptoms and imaging shows significant compression, laminectomy offers posterior decompression of the canal. It removes part or all of the lamina of one or more vertebrae to enlarge the space around the cord, sometimes combined with fixation if stability is needed. Indication is personalised after clinical assessment, neurological exam and imaging.
What is Cervical laminectomy?
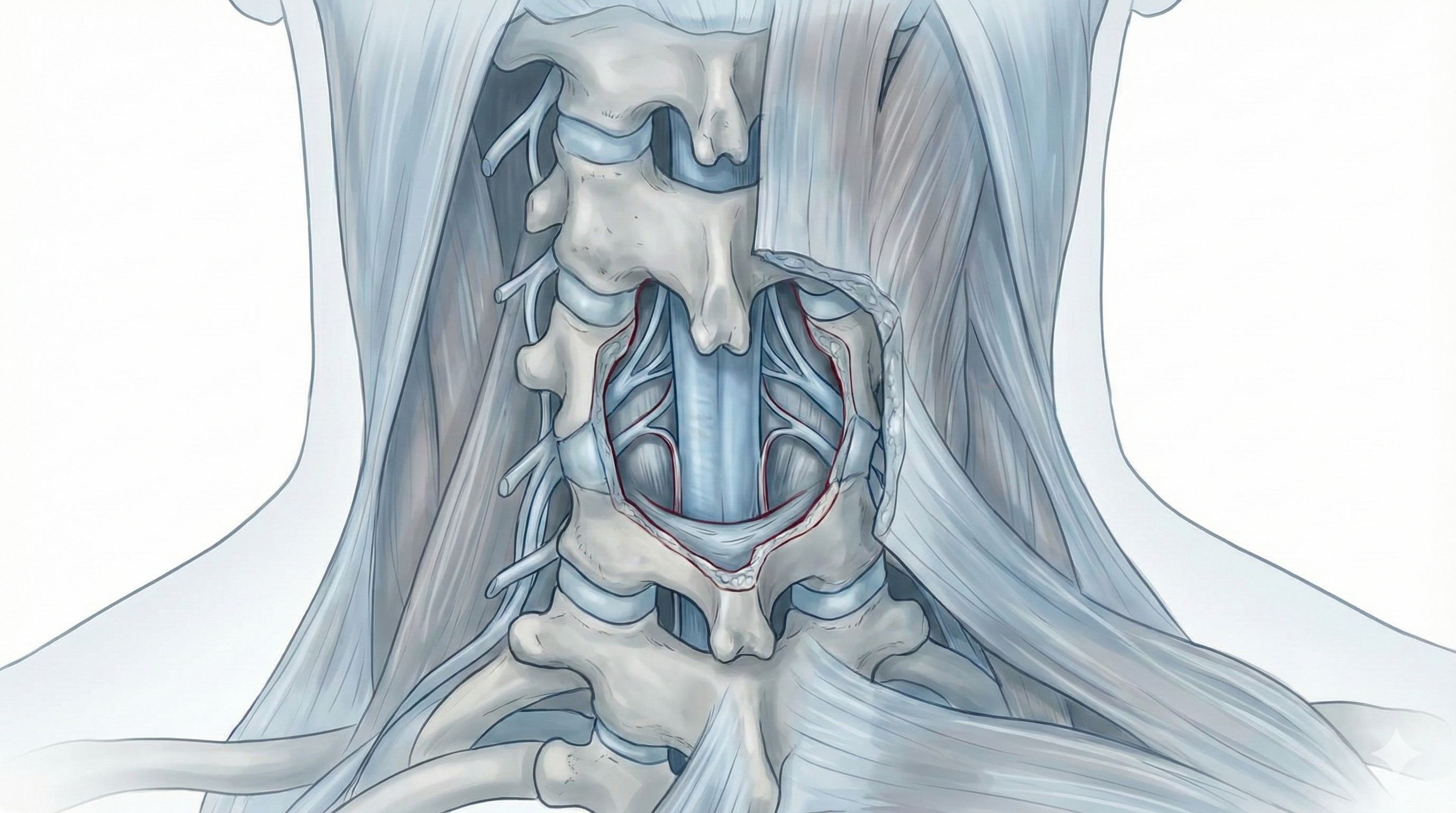
Cervical laminectomy is a surgical procedure in which part or all of the lamina of one or several cervical vertebrae is removed to enlarge the spinal canal and create more space for the spinal cord and nerve roots. It is performed from the back of the neck through an incision and careful muscle separation. The procedure targets the posterior structures of the cervical spine (laminae, ligaments and posterior canal). Its main goal is to decompress the cord and roots when significant stenosis is caused by arthritis, thickened ligaments, posterior disc herniations or other degenerative changes. Unlike anterior approaches with discectomy and fusion, cervical laminectomy tackles the problem from behind and is used when compression is extensive or multilevel. Fixation and fusion may be added if stability is needed.
Symptoms and warning signs
People who may benefit from cervical laminectomy usually show signs of spinal cord or cervical nerve root compression:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
Before cervical laminectomy, a full clinical assessment is performed, including detailed neurological examination and imaging review. The neurosurgeon explains goals, benefits and risks, and answers questions. Fasting instructions are provided and medication is adjusted, especially blood thinners or antiplatelets. Hospital admission is planned and informed consent is signed once everything is clarified.
2.During the procedure
Cervical laminectomy is performed under general anaesthesia through a posterior approach. After the incision, muscles are carefully separated to expose the laminae. Part or all of the lamina and sometimes ligamentum flavum are removed to enlarge the canal and free the cord and roots. Depending on the case, screws and rods may be added to stabilise the spine. Muscles and skin are then closed.
3.Immediate postoperative period
After surgery, the patient stays in recovery to monitor awakening, breathing and pain control, then returns to the ward. Mobilisation starts progressively, usually the next day, beginning with getting up and short walks. Strength, sensation, gait and pain are monitored. Typical hospital stay is 2–3 days, tailored to each patient.
Recovery and daily life
In the first days after cervical laminectomy, neck pain, stiffness and fatigue are common. Basic mobilisation starts early and increases gradually. Return to office work is often considered between 4 and 6 weeks if recovery is favourable; physical jobs involving lifting or forced neck postures usually require 8–12 weeks or more. Physiotherapy, progressive strengthening of neck and back muscles and good daily ergonomics are key. If fever, severe uncontrolled pain, new weakness, worsening gait or any alarm sign appears, seek prompt medical review.
Risks and possible complications
As with any spine surgery, cervical laminectomy carries risks, although most patients recover without major complications. General risks include anaesthesia-related problems, wound infection, bleeding, haematoma and venous thrombosis. Specific risks include nerve root or spinal cord injury, persistence or lack of neurological improvement, residual or chronic neck pain, instability if too much bone is removed without adequate fixation, and long-term changes in cervical alignment. Shoulder or posterior muscle pain related to the approach may also occur. These risks are weighed against the benefit of decompressing the cord and roots in each individual case.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala