Cervical disc arthroplasty (cervical disc prosthesis)
Cervical disc arthroplasty (cervical disc prosthesis) is a surgical option for patients with neck pain, stiffness and arm symptoms due to disc herniation or degeneration. The damaged disc is removed and replaced with a mobile prosthesis to decompress the nerve or spinal cord while maintaining disc height and some motion at the segment. It is considered when medication, physiotherapy or posture changes are no longer sufficient and preserving cervical mobility is desirable instead of fusing the level. Indication is always personalised, guided by clinical assessment and imaging, with clear discussion of expected benefits, recovery and risks.
What is cervical disc arthroplasty (cervical disc prosthesis)?
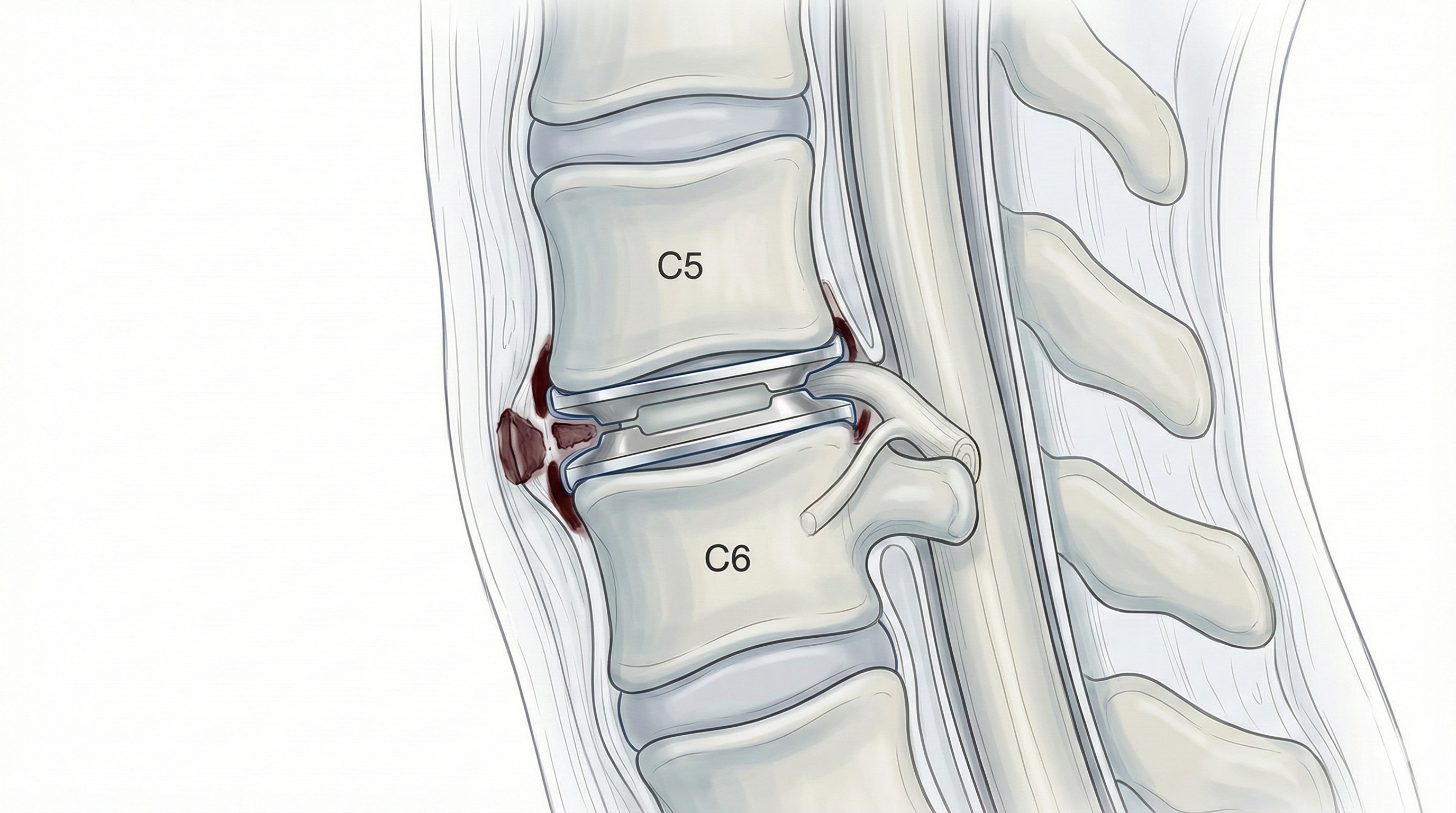
Cervical disc arthroplasty (cervical disc prosthesis) is a surgical procedure in which a damaged or herniated cervical disc is removed and replaced with a mobile prosthesis designed to maintain disc height and segment motion. The approach is usually through a small incision at the front of the neck, gently moving surrounding structures to reach the cervical spine. During the procedure, the surgeon works on the intervertebral disc and the nerve roots exiting the spinal cord in the cervical region. By removing the diseased disc and inserting the prosthesis, the goal is to decompress the nerve or spinal cord while preserving as much natural movement as possible at that level. Unlike anterior cervical fusion, where the segment is fixed and loses motion, cervical disc arthroplasty (cervical disc prosthesis) aims to decompress and preserve movement at the same time, which may help reduce the load on neighbouring levels in carefully selected patients.
Symptoms and warning signs
Patients who may benefit from this procedure usually present symptoms related to cervical nerve root or spinal cord compression. Recognising them and discussing them with a specialist is important. Typical symptoms include:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
Before cervical disc arthroplasty (cervical disc prosthesis), a thorough clinical assessment is carried out, including medical history, current medication and imaging. The specialist explains the procedure, expected benefits and potential risks in detail, and answers all questions. Fasting instructions, medication adjustments (for example, blood thinners) and admission recommendations are provided. The informed consent is signed once everything has been clearly discussed.
2.During the procedure
The surgery is performed under general anaesthesia through a small incision at the front of the neck. The surgeon carefully reaches the affected cervical level, removes the damaged disc and decompresses the nerve root or spinal cord. Then, a cervical disc prosthesis is inserted to restore disc height and allow controlled motion. Intraoperative imaging and other tools are used to ensure correct implant positioning and adequate decompression.
3.Immediate postoperative period
After surgery, the patient spends some time in the recovery room while waking from anaesthesia and having pain controlled. Later, they return to the ward, where gentle mobilisation usually starts within hours. Strength, sensation and neck/arm pain are closely monitored. Hospital stay is typically short, around 24–48 hours, and always tailored to each patient’s clinical situation.
Recovery and daily life
In the first few days after cervical disc arthroplasty (cervical disc prosthesis), it is normal to feel neck discomfort and some stiffness. Basic mobilisation (getting up, walking short distances) is usually started early, following the medical team’s instructions. Returning to office-based work is often possible within 2–4 weeks, while jobs that involve heavy lifting or repetitive neck movements may require 6–8 weeks or more, depending on recovery. Specialised physiotherapy, workplace ergonomics and healthy habits (progressive strengthening, avoiding smoking, weight control) are key to a good outcome. If fever, severe uncontrolled pain or new neurological symptoms appear, it is important to contact the specialist promptly.
Risks and possible complications
As with any surgery, cervical disc arthroplasty (cervical disc prosthesis) carries risks, even though most patients recover without major complications. Knowing these risks helps you make an informed choice. General risks include anaesthesia-related problems, wound infection, bleeding, haematoma and venous thrombosis. Specific risks of this procedure include nerve root or spinal cord injury, temporary swallowing difficulties, irritation or injury to nearby structures (trachea, oesophagus, vessels), implant malposition or wear, bone formation around the prosthesis that may limit movement, and possible degeneration of other levels over time. Although these complications are uncommon, they must always be weighed against the potential benefit of pain relief and functional improvement in each individual case.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala