Cervical corpectomy (removal of one or more vertebral bodies)
Cervical corpectomy (removal of one or more vertebral bodies) is considered for patients with severe neck pain, stiffness and arm symptoms, sometimes with spinal cord involvement causing gait instability. When medication, physiotherapy or injections are no longer enough and imaging shows significant compression, this surgery allows wide decompression of the spinal cord and nerve roots. It involves removing part or all of one or several vertebral bodies with adjacent discs, then placing a cage or graft and a plate with screws to stabilise the spine. Indication is personalised, based on clinical history, neurological exam and imaging, with clear discussion of expected benefits, recovery and risks before deciding.
What is cervical corpectomy (removal of one or more vertebral bodies)?
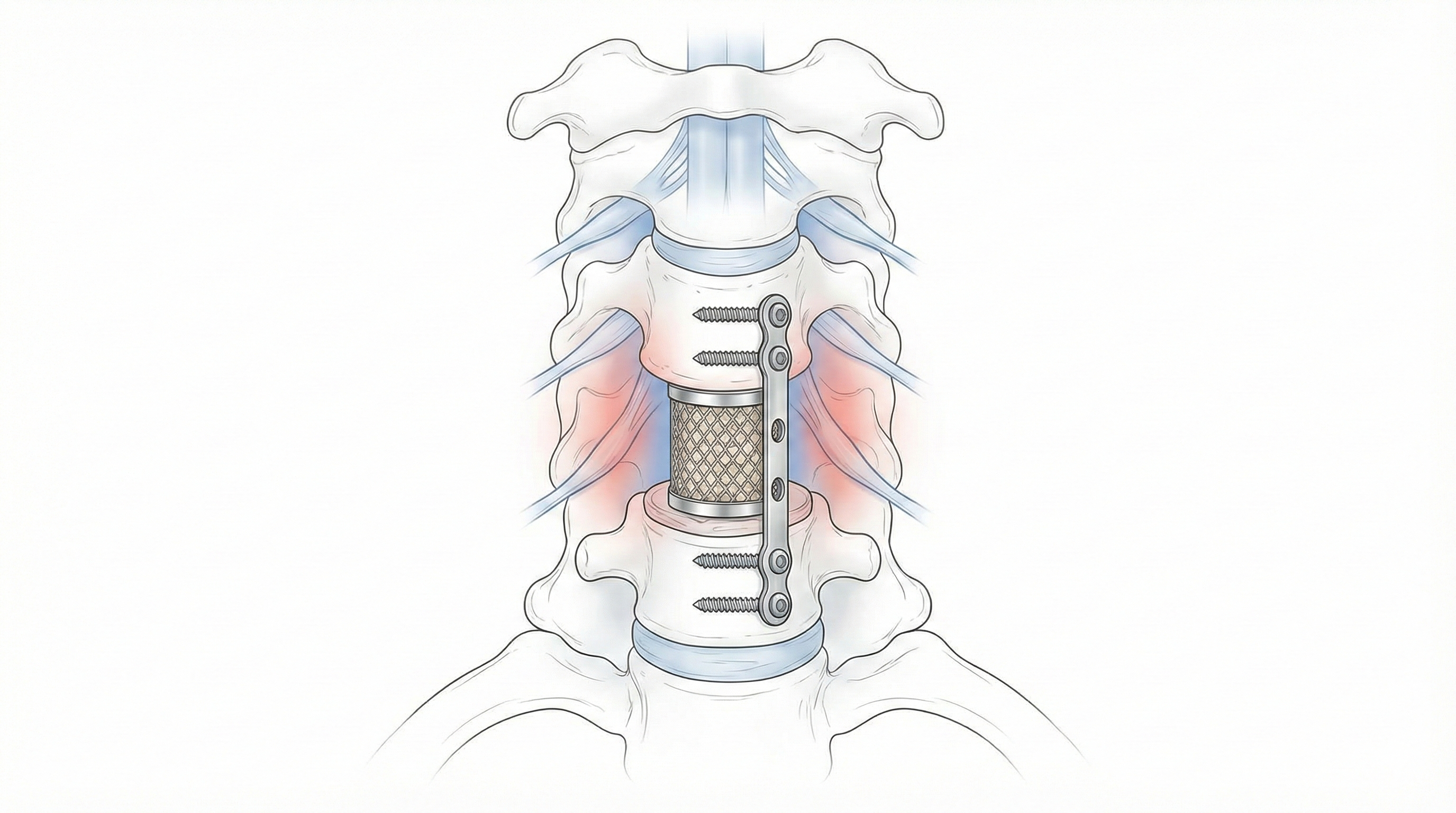
A cervical corpectomy (removal of one or more vertebral bodies) is a surgical procedure in which part or all of one or several cervical vertebral bodies, together with the adjacent discs, are removed to achieve wide decompression of the spinal cord and nerve roots. After bone removal, a cage or structural graft and a plate with screws are placed to stabilise the spine. The procedure acts directly on the front of the cervical spine (vertebral bodies, intervertebral discs and spinal canal). The goal is to create more space for the spinal cord and nerve roots when there is severe compression due to large disc herniations, bone spurs, fractures or deformities. Compared with more limited techniques such as simple discectomy or some posterior decompressions, cervical corpectomy (removal of one or more vertebral bodies) allows a broader decompression of the cervical canal and is usually combined with a solid fusion and stabilisation of the treated segment.
Symptoms and warning signs
Patients who may benefit from a cervical corpectomy (removal of one or more vertebral bodies) often present progressive or intense symptoms related to spinal cord or cervical nerve root compression. Recognising these signs early is important:
When is this procedure indicated?
How is the procedure performed?
1.Preoperative preparation
Before cervical corpectomy (removal of one or more vertebral bodies), a full clinical assessment is carried out, including medical history, detailed neurological examination and review of imaging. Treatment options, reasons for recommending this surgery, and expected risks and benefits are discussed with the patient. Fasting instructions are given, medication is reviewed and adjusted (especially blood thinners), and hospital admission is planned. Once questions are answered, informed consent is signed.
2.During the procedure
Surgery is performed under general anaesthesia through an anterior approach to the neck. The surgeon gently moves neighbouring structures aside to reach the cervical spine. The affected disc and vertebral body or bodies are removed, freeing the spinal canal and compressed nerve roots. A structural device (such as an interbody cage or bone graft) is then placed to fill the bone defect, and a plate with screws is fixed to the healthy vertebrae above and below to provide stability and promote fusion. Intraoperative imaging is used to confirm correct implant positioning.
3.Immediate postoperative period
After surgery, the patient spends a few hours in the recovery room, where awakening from anaesthesia, breathing and pain control are monitored. Afterwards, the patient returns to the ward, where progressive mobilisation usually starts the next day. Strength, sensation, balance and neck/arm pain are closely monitored. Hospital stay is commonly 2–3 days, but it may vary depending on case complexity and individual recovery.
Recovery and daily life
In the first days after cervical corpectomy (removal of one or more vertebral bodies), it is normal to experience neck pain, tightness and general fatigue. Basic mobilisation (getting out of bed, walking short distances, going to the bathroom) usually begins early, following the medical team’s instructions. Returning to office-based work is often considered between 4 and 6 weeks, if recovery is favourable. For jobs involving physical effort, lifting, prolonged driving or forced neck postures, the recovery time is usually longer, often 8–12 weeks or more, depending on the case. Guided physiotherapy, proper posture, progressive strengthening of neck and back muscles and healthy lifestyle habits (weight control, avoiding smoking) are key to good outcomes. If alarm signs such as fever, intense uncontrolled pain, new neurological deficits or severe gait problems appear, it is important to contact the specialist promptly.
Risks and possible complications
As with any spine surgery, cervical corpectomy (removal of one or more vertebral bodies) carries risks, although most patients recover without serious complications. Knowing them helps you weigh the decision more calmly. General risks include anaesthesia-related problems, wound infection, bleeding, haematoma formation and venous thrombosis. Specific risks of this procedure may include nerve root or spinal cord injury, temporary swallowing difficulties, hoarseness due to irritation of the laryngeal nerve, injury to nearby structures (trachea, oesophagus, vessels), loosening or breakage of the implants, lack of bone fusion (pseudarthrosis) and accelerated degeneration of adjacent levels. Although these complications are not common, they must always be considered alongside the potential benefit of relieving spinal cord and nerve root compression. The final decision is made individually, after clear discussion between patient and spine surgeon.
Frequently asked questions
Do these symptoms sound familiar?
If you recognise yourself in some of these symptoms and your pain is starting to limit your daily life, we can review your case in a personalised consultation. Dr. Ben Ghezala will assess your clinical history and imaging studies to help you decide the best treatment option for you.
Request a consultation with Dr. Ben Ghezala